How Healthcare Technology Is Helping to Advance Health Equity
Learn how the adoption of digital health technologies is helping advance health equity for patients in the United States.

Today, many Americans have their healthcare services covered by either private health insurance, with plans offered through a broker or an employer, or by public insurance programs like Medicare or Medicaid, which make it possible to receive healthcare services as needed. Unfortunately, over 26 million people in the U.S. do not have health insurance, making it difficult to receive preventive care or treatment for illnesses and chronic diseases.
Social and economic inequalities disproportionately impact access to healthcare. These health disparities can be caused by economic factors, limited access to housing and transportation, education levels, food insecurity, and other issues in the local community, often referred to as social determinants of health (SDOH).
In order to address the impact of SDOH on health outcomes, the first step is to acknowledge and capture this data in conjunction with patient care. Unfortunately, it can be daunting to capture SDOH data because common healthcare tools like electronic health records (EHR) include fields that were designed primarily to record standard vital sign measurements and other medical information about the patient. If SDOH data is captured at all, it is often manually entered in an open text field, making it difficult to aggregate and analyze this data to identify trends.
In a recent Health Equity Series hosted by the National Health IT Collaborative for the Underserved (NHIT), experts from Docusign, Salesforce, AWS, Veteran Services of Carolinas, and others came together to discuss these issues.
Disconnected medical records: a key barrier to achieving equitable outcomes
Many patients face SDOH-related circumstances that require treatments and interventions from a range of various community support services. These can include a social case worker, a court officer, a counselor for mental health or substance use disorders, and a housing coordinator for those facing homelessness—just to name a few. Each of these resources relies on different systems of record, making it difficult to track and coordinate care.
Luis Belen, CEO of the (NHIT), described the impact of this disconnected data:
“Clinical providers review the data contained in EHRs but they may not be taking into account other providers who the patient has seen and additional data that those providers may have captured. In such a case, these other data sets, like social determinants, are overlooked. We need to find a way to combine that data and make it actionable to create insights that meet the patients where they are. Once you combine health and social determinants data, the question is: do those patients have food insecurities? Do those patients lack broadband access? There’s a lot of disparate patient data in the cloud. But can you actually draw prescriptive insights where you could have a meaningful impact in the patient's lives?”
To address this challenge, NHIT launched the Data Fusion Center, a platform that pulls together and ingests publicly available de-identified data sets that allow for a granular understanding of SDoH and its rippling impacts.
How technology can help address health inequality
Innovative technology solutions are enabling practitioners to address this issue in new ways. For example, Veterans Services of the Carolinas uses a predictive analytics solution to better understand an individual’s risk for homelessness.
The organization used sources such as insurance claim data, geospatial data and social media data to create targeted intervention programs that address and even help prevent homelessness. For example, this type of data allows them to effectively allocate resources and improve veterans' access to food banks to combat the risk of malnutrition.
There's a dire need for interoperable tools that work across existing systems and serve the entire care continuum, rather than just one facet. A 2023 survey by Gartner and Docusign found that 85% of health equity leaders believe digitizing the patient experience leads to better outcomes and improved patient trust.
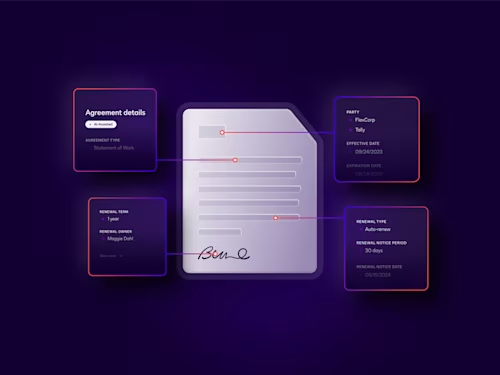
Infor Cloverleaf, an interoperability solution provider, has partnered with Docusign to help address these complex challenges. By digitizing patient intake forms and other related documents, patients can easily complete and submit the necessary agreements in advance via email or on any mobile device. Once completed, the information is automatically updated to the appropriate patient record in their provider’s EHR. This allows the clinicians and staff to focus more on patient care during the visit, instead of exchanging and managing additional paperwork. Lastly, these innovative joint solutions can help achieve secure data exchange at scale between different EHR systems and eliminate the silos that arise when treatments are delivered from multiple service providers.
An improved patient experience builds trust and leads to better outcomes
Trust takes time to earn, but modern, digital healthcare solutions can help bridge the gap between patients and providers—and drive more positive patient outcomes.
Improving the patient experience, particularly digitizing the cumbersome paperwork and automating business processes required for patients and providers, could be a promising first step toward closing the healthcare outcomes gap—and a cost-effective way to help solve the overall puzzle. Here are a few ways that improving productivity through integrated end-to-end document management can eliminate some of the major administrative roadblocks faced by patients today.
Increasing providers’ ability to deliver value-based care for diverse populations, both holistically and affordably, without compromising the quality of care, opens the door to new service models and improved outcomes. For instance, when the pandemic hit, Hospice Savannah quickly sprung into action. When local vaccine sites became overwhelmed with volume, the organization teamed up with the Georgia Department of Public Health to help vaccinate seniors, their caregivers and first responders. Digitizing their agreement process enabled Hospice Savannah to inoculate nearly 1,000 individuals per day while keeping patients and staff safe with contactless, automated and error-free administrative workflow.
Digital patient onboarding and remote healthcare portals—both direct features of advanced digital agreement solutions—provide patients with a frictionless healthcare experience and greater access to care. It makes visiting or communicating with healthcare providers easier and more direct than ever before—and provides patients with a more transparent healthcare experience.
The path forward to advance health equity
As we continue to dismantle barriers and better understand the complex factors that contribute to health equity, it’s also time to consider how technological solutions can improve inclusivity throughout the healthcare system—from the inside out.
Learn more about how Docusign works with healthcare organizations to support this transformation.
Related posts
Docusign IAM is the agreement platform your business needs


