Accelerate Medicaid Access and Transform Recipient Experiences with Docusign
As each state operates its own Medicaid program under federal guidelines, it's time for states to use technology as an enabler for delivering better service.

Medicaid and CHIP currently provide health and long-term care benefits for over 93 million people, about 21% of the U.S. population. Considering over 61% of adults covered are employed and 60% of non-elderly Medicaid enrollees are people of color, there are complex economic, accessibility and other social determinants to consider when striving to deliver equitable experiences for all beneficiaries.
Many applicants and enrollees cope with economic hardships while working low-paying jobs. Taking the time to visit a physical office to apply for Medicaid benefits can be a daunting challenge for many who also lack adequate access to transportation. In addition, Medicaid enrollees may not have access to computers in their homes and have to manage multiple complex processes—from eligibility determination to claim submission—from their mobile devices.
As each state operates its own Medicaid program under general federal guidelines, now’s the time for states to consider technology as an enabler for delivering better service and meeting the needs of all Medicaid members.
The complexity of today’s Medicaid experience
The full Medicaid experience spans multiple interdependent processes and workflows, both before and after the actual delivery of care.
Several high-profile initiatives, starting with the expansion of Medicaid under the Affordable Care Act (ACA), have proven consequential to this experience. Most recently, Medicaid coverage was expanded to nearly all adults with incomes up to 138% of the Federal Poverty Level, equivalent to $20,120 for an individual in 2023.
Additionally, the practice of continuous enrollments due to the Families First Coronavirus Response Act (FFCRA) has been discontinued. These enrollments ended on March 31, 2023, and the related processes have been known as the “unwinding” of Medicaid. Medicaid enrollees face several challenges during this unwinding, and the Kaiser Family Foundation (KFF) estimated that between 8 million and 24 million people would lose Medicaid coverage as a result.
The Medicaid redetermination process is also presenting a new set of challenges for state Medicaid agencies due to record levels of re-enrollments, which must be managed efficiently to ensure there are no gaps in health coverage for those in need.
Furthermore, as states unwind the continuous enrollment provision throughout the subsequent 12 months, they’ll also redetermine eligibility for all current Medicaid enrollees and disenroll those no longer eligible. This includes individuals who may remain eligible but cannot complete the renewal process in time due to unsuccessful outreach attempts after a change in address, etc.
Many states are making strides in the right direction while needing help with legacy systems and outdated, manual processes. For example, 44 states now allow individuals to upload verification documents online and have digitized outbound member notices. However, only 32 states offer mobile-friendly formatting for their online Medicaid enrollment processes and related applications.
Navigating the Medicaid experience can be complex. The key is to provide an equitable experience for all current and potential Medicaid enrollees through paperless processes that lead to more timely access to care and improved outcomes.
Enhancing Medicaid recipient experiences
Docusign defines and builds user experiences around engagement, efficiency and effectiveness. This three-pronged approach can help any state Medicaid agency meet the needs of Medicaid beneficiaries, clinicians, and community service providers.
Engagement
To better deliver long-term services, organizations strive to create more intuitive interactions for applicants who are communicating with Medicaid agencies and physicians who are interfacing with their provider portals. This is achieved through faster enrollment and verification workflows and improved accessibility, thereby optimizing the coordination of care.
For example, Docusign eSignature and Web Forms allow applicants to easily complete and sign forms electronically and upload supporting documentation, reducing the time it takes to satisfy such requirements. This accelerates enrollment and the eligibility review process thanks to the secure, dynamic form-filling experience. The mobile-friendly features also make the information more accessible to a broader range of collaborating stakeholders, improving the overall user experience for everyone.
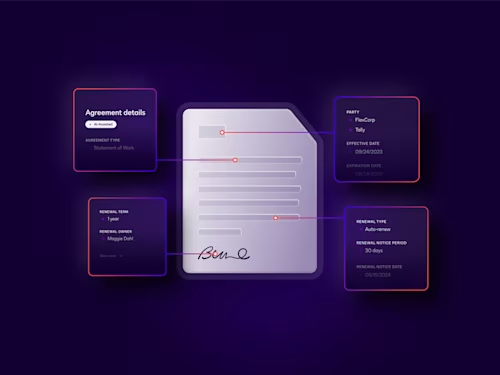
Medicaid programs depend on an extensive network of healthcare providers, and Docusign solutions help simplify the management of the provider lifecycle, including contracting and onboarding. As providers renew terms, update services offered or change other details, these adjustments are digitally captured and confirmed with a legal signature—all through an automated workflow users can access from almost anywhere on any device.
Efficiency
Enhanced efficiency boils down to being able to streamline access to care, as well as optimize administrative agency back-office processes. This includes automating manual workflows and aggregating disparate repositories to securely create a single source of truth. Essentially, efficiency is achieved through the optimization of the processes that sit behind the metaphorical curtain.
From enrollment forms to claims adjudication and provider contracts, Medicaid has traditionally relied on a lot of cumbersome paperwork. With Docusign solutions, agencies can deliver digital-first experiences, which can reduce risk and accelerate the submission and review of documents.
Medicaid administrators and providers can now offer a digital intake process for both remote and in-person interactions with Docusign. This makes it possible to automatically send patient consent forms and other intake documents from the EHR to patients via SMS or email—without any staff intervention.
Effectiveness
Effectiveness is the accurate measure of impact from investments and efforts employed to improve user engagement and back-office efficiency while also correlating improvements to positive shifts in outcomes across these mission-critical programs. This is especially true as value-based reimbursement models are evolving to consider quality metrics like hospital readmission rates, patient satisfaction scores and claims processing times. Reducing errors and maintaining compliance is paramount.
As many Medicaid forms contain personally identifiable information (PII) of applicants and enrollees, it’s critical for agencies and their partners to maintain detailed audit trails of eligibility evaluation documents and chain of custody for claims and appeals.
Docusign eSignature offers built-in features such as required fields and audit trails to help reduce errors and ensure all necessary information is collected, properly routed and securely stored. This helps support compliance with Medicaid program requirements while reducing the risk of fraud.
Get started today
Are you ready to streamline your Medicaid documentation process and efficiently engage with applicants, enrollees and beneficiaries? Start using Docusign today and experience the benefits firsthand. Request a demo today to see how Docusign can transform your Medicaid workflows.
Related posts
Docusign IAM is the agreement platform your business needs


